Stroke care in the United States
Our Mission
We aim to improve the quality of Telemedicine evaluations for acutely ill patients. Telemedicine consults have become the standard of care for acute stroke patients and patients with acute neurological complaints. More than 1000 Acute Telemedicine evaluations are performed across the United States every day. Our experts are developing accessory tools to improve the quality of these evaluations, which in turn will improve patients’ outcomes.
Our Vision
About 50% of acute ischemic stroke cases (which are strokes caused by blood clots in the arteries of the brain) are triaged via telemedicine (close to 200,000 per year). While stroke has a wide spectrum of clinical symptoms, approximately 10-15% of cases present with visual disturbances or abnormal eye movements that can only be detected through ocular-based neurological examination. These are called posterior circulation strokes, which account for 20-25% of all ischemic strokes, and require a Neurologist’s assessment and diagnosis.
Neurology researchers at the University of Toledo have developed a novel Telestroke eye examination device for accurately assessing visual fields and monitoring eye movements without relying on a person at the bedside of the patient. The novel device consists of a custom-made head-mounted eye visor with a camera pointed towards the eyes of the wearer and allows the practitioner to remotely assess a patient’s field of vision without the help of a person to observe the patient’s eye movements. Additionally, a mobile application will aid the practitioner in controlling the cameras, managing light synchronization, collecting live data on eye movement, and serving as a wireless communication between the accessory device and the practitioner. The novel device can also work with existing Telestroke apps and software.
Market Opportunity
Stroke is the 5th leading cause of death in the United States and the leading cause of adult disability. Approximately 795,000 new or recurrent strokes occur every year in the US, with 147,810 individuals dying annually due to stroke. In 2018, stroke accounted for ~1 out of every 19 deaths. By 2030, the prevalence of stroke is projected to increase by 20.5% in the US. Between 2015 and 2035, the total direct medical stroke-related costs are expected to rise from $36.7 billion to $94.3 billion.
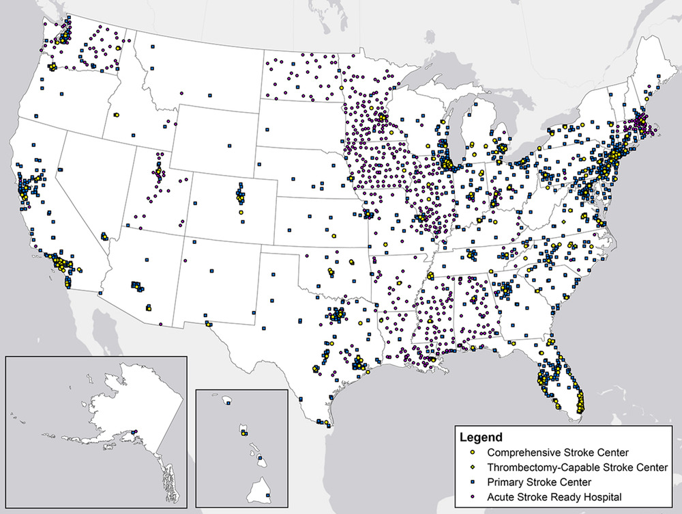
Most often, stroke patients are first seen in emergency departments (EDs). Due to the landscape of healthcare in the United States, which includes many underserved rural areas, approximately 58% of US EDs (as of 2015, there are ~5200 documented EDs in the US) utilize telemedicine systems to evaluate and diagnose patients. Telemedicine allows hospitals to connect with specialists remotely, thus enabling even rural hospitals the ability to provide a higher level of care that may not otherwise be available. Unfortunately, stroke is a condition that cannot be fully assessed and diagnosed with existing remote telemedicine systems.
WHY IT MATTERS.
Stroke is the nation's No. 5 killer and a leading cause of serious long-term disability, with nearly 800,000 strokes. However, not all Americans have equal access to certified stroke centers.
DevelopingEmergingMeet the Team
-

Mouhammad Jumaa, MD
Inventor
Chief Technology Officer
Dr. Jumaa is a board-certified Vascular and Interventional Neurologist with over 10 years of clinical and research experience. His strong interest in pre-hospital stroke diagnosis led him to co-invent our device. Dr. Jumaa has also fostered the development of several apps, which include a second opinion physician-to-physician app (endorsed by the Society of Vascular and Interventional Neurology) and an app to promote the global mission of mechanical thrombectomy utilization growth worldwide.
-

Julie Shawver, PA-C
Project Manager
Julie Shawver is a board-certified Physician Assistant with over 10 years of experience specializing in Neurology and Vascular Neurology. As Stroke Coordinator, Julie Shawver’s expert acute stroke clinical knowledge and skills support the synthesis of project development.
-

Syed Zaidi, MD
Chief Medical Officer
Dr. Zaidi is a board-certified Vascular and Interventional Neurologist with over 10 years of clinical and research experience. He is co-inventor of our device and has also co-designed and launched several apps for the Society of Vascular and Interventional Neurology.